Phase 1 clinical trials occurred in 2,784 instances, accounting for nearly 41 percent of all clinical trials globally, according to recent 2022 data (source). In general, there are more Phase 1 clinical trials than Phase 2 or Phase 3 due to the exploratory nature of drug development.
As we dive deeper into understanding Phase 1 clinical trial designs and bioequivalence (BE)/bioavailability (BA), we learn that the purpose of a Phase 1 Clinical Trial is to evaluate the safety, tolerability, and pharmacokinetics (PK) of an experimental drug. Only when the experimental drug has been tested and approved in preclinical trials (lab or on animals), can it then be tested on humans.
A Phase 1 Clinical Trial is generally conducted on healthy participants only, and just a small number of participants are considered for recruitment, meaning that the sample size is much smaller than other clinical phases. See Figure 1 below for further clarity.
Figure 1. Phases of the Clinical Trial Development
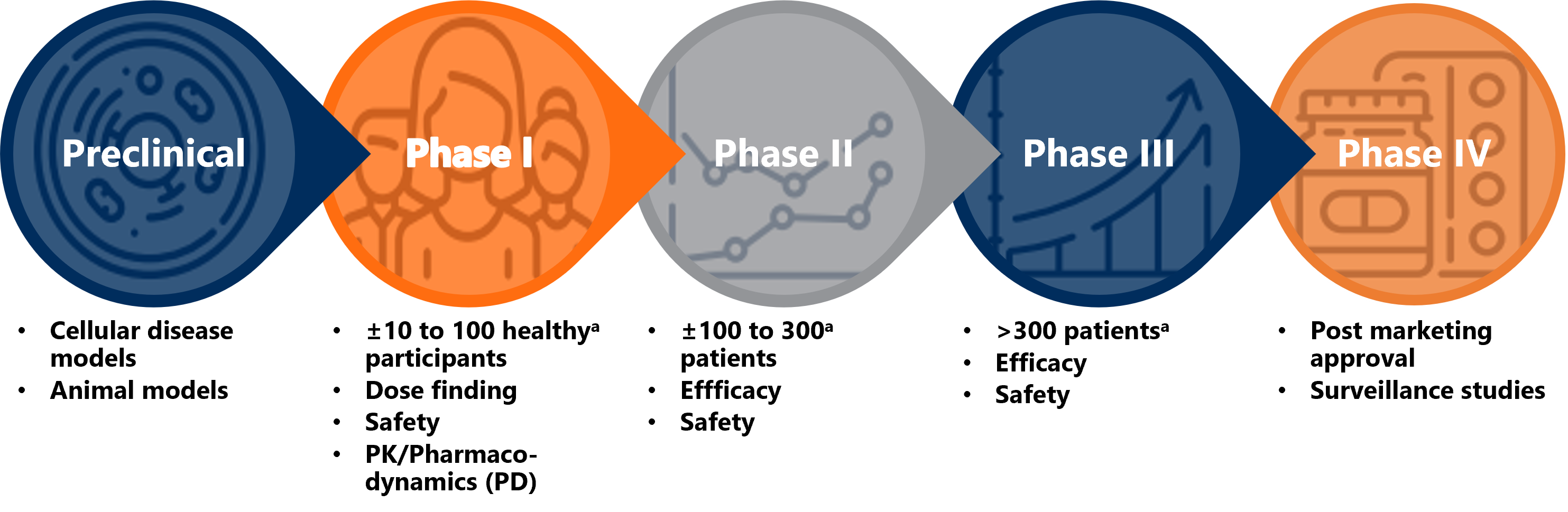
aSample sizes are only an average presentation and can be different based on the therapeutical area and design of the clinical trial.
As a crucial part in the drug development process, many potential new therapies do not make it past the Phase 1 clinical trials stage due to safety and efficacy concerns. Early Phase 1 Clinical Trials can be distributed into several unique Phase 1 trial designs.
Common Phase 1 clinical trial designs
Clinical trial designs, as detailed in Figure 2, commonly used in Phase 1 Clinical Trials are single ascending dose (SAD), multiple ascending dose (MAD), food effect studies, drug-drug interaction studies, and BE/BA clinical trials. Each clinical trial design has its own unique set of objectives and corresponding analyses, but for the purposes of this text, we will focus on BE/BA clinical trials.
Figure 2. Phase 1 Trial Designs

What is BE/BA in Phase 1 clinical trials?
BA is the rate and extent to which the active compound is absorbed from a drug and becomes available to the body. BE, on the other hand, is the absence of a significant difference in the rate and extent to which the active ingredient in an experimental drug and reference drug becomes available at the target site when administered at the same molar dose under similar conditions.
Before we can delve further into how BE/BA is determined, PK must be explained. PK explores how a drug enters, moves, changes, and leaves the body. This is characterized in pharmacology by the acronym ADME, or absorption, distribution, metabolism, and excretion.
Figure 3, below, details an illustrated view of the concentration of a drug within the body over time.
Figure 3. Concentration vs Time Curve
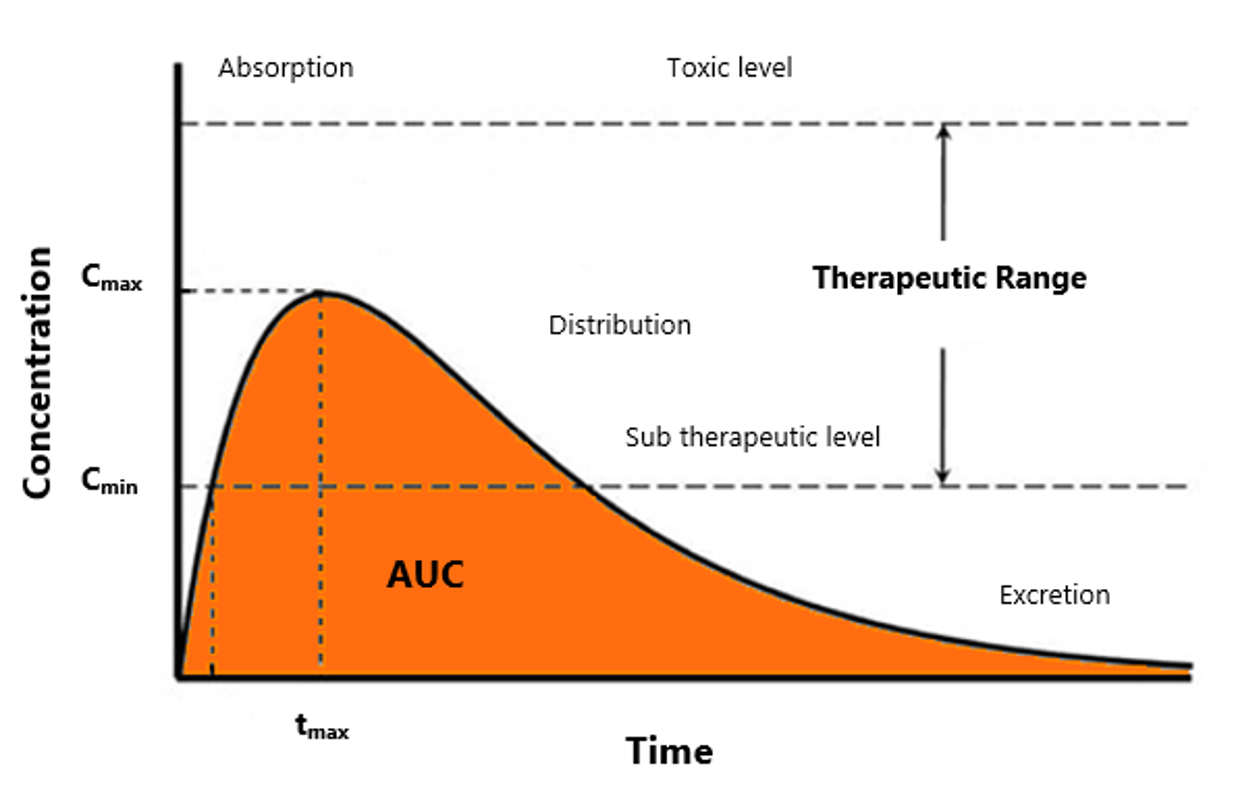
Bioavailability is determined by using three primary PK parameters, which are:
- Area under the concentration-time curve (AUC): This parameter reflects the extent of exposure.
- Maximum concentration (Cmax): This parameter is influenced by the absorption rate.
- Time to maximum concentration (tmax): This parameter indicates the time it takes to reach the maximum concentration.
It is important to note that bioavailability is not assessed via bioequivalence testing, however, bioequivalence is assessed via bioavailability testing.
BE/BA trials are designed in such a way that the compound effect can be distinguished from any other effects. This is achieved by a randomised, crossover design with wash out periods that separate the treatment periods to ensure that drug concentration is below the lower limit of quantification in all participants before they begin with the next period’s administration.
Washout periods should at least be 5 elimination half-lives. A half-life is the amount of time it takes the concentration of a drug to reduce by 50 percent within the body.
The reference and experimental drug are considered bioequivalent when the 90 percent confidence interval (CI) for the log transformed ratio exposure (Cmax and AUC) measure falls within the range 80 to 125 percent. The reference range is based on a decision by regulatory authorities that differences in systemic drug exposure should not exceed 20 percent.
Sponsors should know this about Phase 1 clinical trials in the US
-
- Sample size: Sponsors should determine the adequate number of clinical trial participants, allowing for the potential of dropouts. The adjustment for a dropout should be accounted for in the randomization schedule and clinical study protocol before any randomization is done.
- Consistent logarithmic adjustments: FDA guidance recommends that BE measures be log-transformed. The choice of common or natural logs needs to be consistent and should be stated in the clinical study protocol and statistical analysis plan (SAP).
- Testing for normality: Sponsors are not encouraged to test for normality of error distribution after log-transformation, nor should they use normality of error distribution as a reason for performing statistical analyses on the original scale. Justification should be provided if a Sponsors believes that their BE clinical trial data should be statistically analysed on the original rather than on the log scale.
- Trial Designs: Sponsors should be vigilant about the design of the clinical trial which can be determined by a large variation and carryover effects. When choosing a CRO, Sponsors should be able to trust their support in important decision making and collaborate to determine the best clinical trial design given the nature of the new experimental drug. If carryover effects are evident, the proposed approach should be detailed in the clinical trial protocol, including statistical tests for the presence of such effects and procedures to follow.
European Phase 1 clinical trials
In the European Union (EU), EMA suggests that the selection of the generic or reference drug used in a bioequivalence trial should be based on assay content and dissolution data and is the responsibility of the Sponsor.
It is advised by the EMA that the assayed content of the batch used as experimental drug should be within 5 percent of the reference drug batch determined with the test procedure for routine quality testing of the experimental drug. It is recommended to test more than one batch when selecting a reference drug and the Sponsor should document how a representative batch has been selected based on the assay content.
Another consideration employed by the EMA is the use of urinary excretion data as a substitute for plasma concentration. If it is determined that plasma concentration-time profiles for the active compound cannot reliably be computed, Sponsor may use urinary excretion concentration data, with the necessary justification, to support the extend of exposure.
In European Phase 1 clinical trials, we also see highly-variable drug products (HVDP), whose intra-subject variability for a parameter is larger than 30 percent. A replicate cross-over design trial can be carried out to satisfy EMA requirements regarding highly variable experimental drugs.
Finally, Sponsor in the US and EU need to consult their CRO in order to determine adequate resources to calculate the PK parameters associated with BE clinical trials. These include the type of clinical trial design, whether it is blood plasma or urine concentration data.
When conducting any Phase 1 clinical trial, costs can mount upwards of $6.6 million according to the National Institutes of Health (NIH). In these early stages, Sponsors need to be vigilant around the cost of conducting Phase 1 clinical trials, especially when it comes to the field of pharmacokinetics where the right resources come at a premium. Consulting a trusted clinical research organization for costs and resourcing is highly recommend.
Resources to support your Phase 1 clinical trials journey
For a complete guide to determine bioequivalence in the US, please consider this FDA resource: Statistical Approaches to Establishing Bioequivalence | FDA
For guidelines on the investigation of bioequivalence and statistical approaches in the EU, please consider this EMA resource: Investigation of bioequivalence | European Medicines Agency (europa.eu)
Bioequivalence trials conducted within South Africa must adhere to SAHPRA regulations in conjunction with the FDA and EMA. See Quality and Bioequivalence guideline – SAHPRA for more details.
Please click here to start a conversation with a Phase 1 clinical trial expert or if you have any questions related to this article.
Authored by: Paul Meades, Associate Manager, Biostatistics.

